A new neuroimaging study comparing brain activity of depressed people suffering from insomnia with brain activity of people without insomnia has found that participants with insomnia and depression had higher resting-state functional connectivity in the superior temporal gyrus region of the brain on both sides. This type of connectivity was decreased in the left supplementary motor area and bilateral postcentral gyrus regions of the brain. The study was published in Psychiatry Research: Neuroimaging.
Depression (or major depressive disorder) is a mental health disorder characterized by persistent and intense feelings of sadness, hopelessness, and a loss of interest or pleasure in activities that were once enjoyable. It is a third leading cause of disability worldwide. Depression adversely and substantially affects the quality of life of people suffering from it and imposes a heavy burden on the community.
One of the most common physical symptoms found in patients with depression is insomnia. Insomnia is characterized by difficulty in falling asleep, staying asleep, or waking up too early and not being able to go back to sleep. Studies have shown that 92% of patients with major depression have problems with sleep, with 85% fulfilling criteria for insomnia.
Neuroimaging studies have indicated that the development of depression is associated with abnormalities in the functioning of brain regions involved in emotional processing and regulation. Identifying regions of the brain and brain activity patterns involved in specific symptoms of depression thus became a topic of intense scientific inquiry.
Study author Yanxiang Ye and his colleagues wanted to explore the brain processes underlying insomnia in patients with major depressive disorder. They focused their attention on the amygdala region of the brain and conducted a study using functional magnetic resonance imaging to study patterns of activity in this region.
There were two groups of participants – 102 patients suffering from the major depressive disorder and 57 healthy individuals used as controls. The researchers assessed the presence of sleep disturbances (a subscale of the Hamilton Depression Rating Scale) and divided further into two groups – high insomnia and low insomnia, depending on how pronounced they reported sleep disturbances to be.
Forty-six of these patients formed the high insomnia group and 56 the low insomnia group. All patients were undergoing treatment at the Affiliated Brain Hospital of Guangzhou Medical University.
Participant underwent functional magnetic resonance imaging at the Affiliated Brain Hospital of Guangzhou Medical University using a 3.0-Tesla Philips Achieva scanner. The researchers recorded resting state brain activity i.e., participants were asked to lay still and stay awake with their eyes closed during brain imaging.
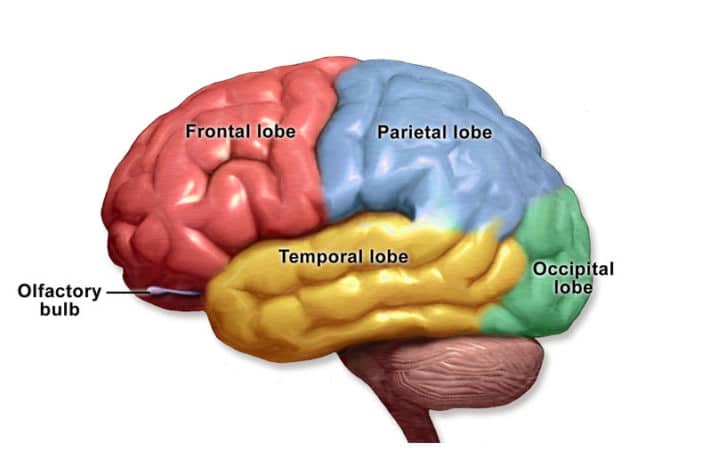
Results showed that the high insomnia group had higher activity in the left calcarine and superior temporal gyrus regions of the brain compared to both healthy participants and the low insomnia group. The three groups also showed different levels of brain activity at rest in bilateral superior temporal gyrus, left middle temporal gyrus, left supplemental motor area, and bilateral postcentral gyrus regions.
Of these, the high insomnia group had increased activity in the superior temporal gyrus, while the low insomnia group had increased activity in the left supplemental motor area and the bilateral postcentral gyrus regions compared to healthy participants.
An association between functional connectivity of bilateral amygdala to the superior temporal gyrus regions and the intensity of sleep disturbance was found. Greater connectivity in this area was linked with higher levels of sleep disturbance.
The superior temporal gyrus is a region of the brain located in the temporal lobe, which is involved in auditory processing, language comprehension, and memory. It plays a critical role in speech perception, and damage to this area can cause difficulty in understanding speech.
The amygdala, on the other hand, is a small almond-shaped structure located deep in the temporal lobe of the brain. It plays a key role in processing and regulating emotions, particularly fear and anxiety. The amygdala is responsible for detecting potential threats in the environment and initiating the “fight or flight” response to keep the individual safe.
“Our findings suggest that resting state functional connectivity in temporal lobe and other specifically activated regions may be associated with neural circuits involved with insomnia in major depressive disorder,” the study authors concluded.
The study gives an important contribution to the scientific understanding of neural correlates of insomnia in people with depression. However, it should be noted that the study was not able to provide data on how these changes develop. It is also unclear whether the observed changes in brain activity are the cause of the lack of sleep or a manifestation of the fact that participants are not getting enough sleep.
The study, “Abnormal amygdala functional connectivity in MDD patients with insomnia complaints”, was authored by Yanxiang Ye, Chengyu Wang, Xiaofeng Lan, Weicheng Li, Ling Fu, Fan Zhang, Haiyan Liu, Zhipei Zhang, Kai Wu, Yanling Zhou, and Yuping Ning.
