A new study published in NeuroImage: Clinical explored the relationship between exercise, brain functioning, and major depressive disorder. The findings indicate that individuals with major depressive disorder (MDD) who also exercise tend to have better brain functioning than those with MDD who do not exercise.
Depression is a common mental health disorder that affects millions of people worldwide. It is characterized by persistent sadness, hopelessness, and loss of interest in once enjoyable activities.
Depression can significantly impact an individual’s quality of life, affecting their ability to work, socialize, and carry out daily activities. Physical exercise has been shown to be an effective treatment for depression, with studies suggesting that it can improve mood, reduce symptoms of depression, and enhance cognitive functioning.
“To develop optimized physical exercise treatments that serve as clinically useful additional treatment options for MDD, it is important to gain a better understanding of biological mechanisms of physical activity and their effect on cognitive functions and depressive symptoms,” wrote the authors of the new study.
“Therefore, as a first step, this cross-sectional study is focused on physical activity and individual physical fitness without an intervention. It is thought that antidepressive effects of increased physical activity and fitness are mediated by neuroplasticity that supports cognitive functioning.”
The study recruited 111 MDD outpatients and 56 healthy control (HC) participants. Participants had to engage in less than 90 minutes of vigorous physical exercise per week to be included in the study. Participants underwent tests to assess their physical fitness and neural activity during working memory performance.
Physical fitness was assessed using a graded exercise test on a cycle ergometer, where participants completed an electrocardiogram (ECG) during bicycle ergometry to measure their maximum physical exertion. Neural activity was measured using functional magnetic resonance imaging (fMRI) during a working memory task.
Participants with MDD had lower performance and slower response times on a working memory task compared to healthy individuals. The difficulties were especially prominent when the task required higher mental effort.
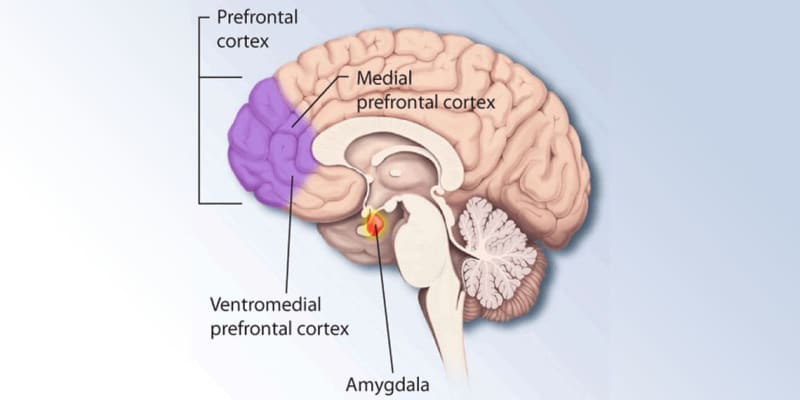
Brain scans showed reduced activity in certain regions of the brain associated with working memory in MDD patients. However, higher levels of physical fitness were associated with increased neural activity in the prefrontal cortex during working memory performance in individuals with MDD, suggesting that higher fitness levels may help improve working memory function in MDD.
The findings from this study provide valuable insights into the benefits of exercise for individuals with depression. The results suggest that physical fitness may enhance cognitive functioning in individuals with MDD by increasing neural plasticity in the brain. This has important implications for the treatment of depression, as it suggests that exercise may be an effective adjunct therapy for individuals with depression.
One limitation of this study is the small sample size and cross-sectional design of the study, which may limit the generalizability of the findings. Additionally, the study excluded individuals who exercise more than 90 minutes a day, potentially leaving out data that may be meaningful to the study of how exercise intersects with major depressive disorder.
“To our knowledge, this is the first study dedicated to the relationship between functional brain activity in a [working memory] task and physical fitness in MDD,” the researchers said. “The present results can be used to guide future research on physical fitness or exercise effects on mental health and cognition to develop optimized physical exercise treatments that serve as clinically useful additional treatment options for MDD.”
The study, “Physical fitness is associated with neural activity during working memory performance in major depressive disorder,” was authored by M.K. Schwefel, C. Kaufmann, G. Gutmann, R. Henze, T. Fydrich, M.A. Rapp, A. Ströhle, A. Heissel, and S. Heinzel
