A temporary increase in stress hormones appears to play a key role in reducing anxiety-like behaviors in mice that have been administered the psychedelic substance psilocybin. The findings, published in ACS Pharmacology & Translational Science, provide new insights into the underlying mechanisms that may be involved in psilocybin-assisted psychotherapy.
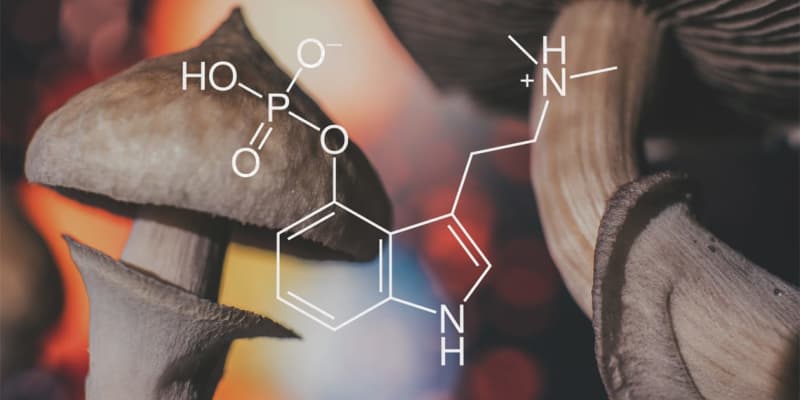
Psilocybin is a naturally occurring psychedelic compound found in certain species of mushrooms, often referred to as “magic mushrooms.” When ingested, psilocybin is converted into its active form, psilocin, in the body. Psilocin primarily interacts with serotonin receptors in the brain, particularly the serotonin 2A receptor subtype. This interaction leads to altered perception, mood, and consciousness, resulting in a psychedelic experience.
Psilocybin-assisted psychotherapy is a therapeutic approach that involves administering a controlled dose of psilocybin to individuals under the guidance of trained therapists. The therapy session typically includes psychological preparation, the administration of psilocybin in a supportive environment, and post-session integration. The therapist helps the individual navigate their psychedelic experience, providing emotional support and guidance to explore and address underlying psychological issues or challenges.
This form of psychotherapy has gained attention in recent years due to its potential to treat various mental health conditions, including substance use disorders, end-of-life anxiety, major depressive disorder, and treatment-resistant depression. However, there is still much to learn about the mechanisms involved in this therapeutic process.
The authors of the new study aimed to better understand the role of stress-associated hormones in the effects of psilocybin. There is evidence suggesting a correlation between acute cortisol release, anxiety, and therapeutic outcomes with psilocybin. But it is unclear whether cortisol release is a necessary factor for the anxiolytic (anxiety-reducing) effects of psilocybin.
“Psychedelics like psilocybin are being increasingly explored in human clinical trials as a means to support non-drug, talk therapy approaches for disorders like depression, anxiety, addiction, and post-traumatic stress disorder,” said study author Cody J. Wenthur, an assistant professor and Director of Psychoactive Pharmaceutical Investigation Programs at the University of Wisconsin–Madison. “As these compounds move ever closer to review by the FDA for clinical use, getting a better idea of how they work on a biological level is critical for the design of protocols that maximize safety and minimize risk.”
To better understand the molecular effects of psilocybin independently of psychological support, the researchers turned to animal models, allowing them to investigate the biological and pharmacological aspects of psilocybin without the complexity of human psychological factors.
The researchers administered psilocybin to male C57Bl6/J mice and examined various behavioral parameters. They also measured the concentration of psilocybin and its active metabolite, psilocin, in the mice’s plasma using mass spectrometry. The study included tests such as the Open Field Test (OFT), the Head Twitch Response, and the Novelty Suppressed Feeding (NSF) assay.
The results of the study revealed several key findings. First, mice administered a specific dose of psilocybin (3 milligrams per kilogram of body weight) exhibited behaviors that resembled the effects of anxiolytic drugs (substances known to reduce anxiety). The effects were noticeable four hours after the mice received the dose. Psilocybin also increased the number of head twitch responses, indicative of its hallucinogenic activity.
One of the key findings of the study was that corticosterone, a hormone associated with the stress response, played a pivotal role in mediating the behavioral effects of psilocybin. When mice were administered psilocybin, it led to a rapid increase in plasma corticosterone levels.
This hormone seemed to be closely linked to the changes in behavior that were observed in the mice following psilocybin administration. In other words, the behavioral effects of psilocybin, such as alterations in anxiety-like behaviors, appeared to be influenced by the release of corticosterone.
To further confirm this relationship, the researchers used a substance called mifepristone, which is known to block or antagonize the receptors for corticosterone. When mice were treated with mifepristone before receiving psilocybin, it effectively prevented the behavioral changes that were typically associated with psilocybin administration.
In addition, when psilocybin was given to mice that already had chronically elevated levels of plasma corticosterone, the long-term anxiolytic effects of psilocybin were lost. In other words, the anxiety-reducing benefits of psilocybin did not occur when corticosterone levels were consistently high.
“Psilocybin causes the release of stress-associated hormones alongside the altered perceptions of reality it causes,” Wenthur told PsyPost. “We found that in mice, this increase in stress-associated hormones was actually helping support reductions in anxiety that lasted for up to one week. Importantly, this was only seen when the increased levels of these hormones was allowed to return to normal. When the levels stayed elevated for the whole week, we saw the opposite effect, a long-term increase in anxiety.”
Interestingly, the researchers also found that similar post-acute anxiolytic effects could be induced by alternative interventions that caused plasma corticosterone increases. Lisuride, a compound with serotonin 2A agonist activity similar to psilocybin but without overt perception-altering effects, also induced anxiolytic-like effects in the NSF assay, indicating that glucocorticoid release alone could produce these effects.
“I was surprised that the effects on anxiety reduction were not changed much by blocking the serotonin 2A receptor, which is one of the main ways that psilocybin causes altered perceptions,” Wenthur said. “This indicates that the activation of a systemic hormonal response may be a complementary, and not fully serotonin-dependent pathway by which psychedelics can support behavioral changes.”
The findings emphasize the importance of considering the role of glucocorticoid release, whether induced by psilocybin or other stressors, as a potential confounding factor in the interpretation of both acute and post-acute effects of psilocybin on anxiety-like behaviors in mice.
But as with all research, the new study includes some caveats. While the study provides insights into the fundamental mechanisms underlying psilocybin’s effects, it remains to be seen how these findings relate to human experiences.
“These experiments were run in mice, not people,” Wenthur said. “While that can help us understand what biological components of the response are important in the absence of preconceived notions or expectations around psychedelics that are often found in people, it does really limit us from understanding how the biology interacts with the psychological and cognitive effects of psilocybin. For that we need to continue working with people, perhaps further exploring changes in cortisol over time as a factor influencing the size and duration of therapeutic responses.”
Wenthur added that Nathan Jones, a graduate student in his lab, played a key role in the study and was the first author on the publication.
The study, “Transient Elevation of Plasma Glucocorticoids Supports Psilocybin-Induced Anxiolysis in Mice“, was authored by Nathan T. Jones, Zarmeen Zahid, Sean M. Grady, Ziyad W. Sultan, Zhen Zheng, John Razidlo, Matthew I. Banks, and Cody J. Wenthur.
