Anorexia nervosa, a severe eating disorder characterized by an extreme fear of weight gain and restricted food intake, has been the subject of increased research to understand its complex neurobiology. A recent study published in Psychological Medicine utilizing robust sample sizes and advanced imaging techniques reveals significant differences in brain connectivity patterns among individuals with anorexia compared to healthy controls. These findings could help in diagnosing and distinguishing different types of anorexia nervosa, potentially leading to better-targeted treatments.
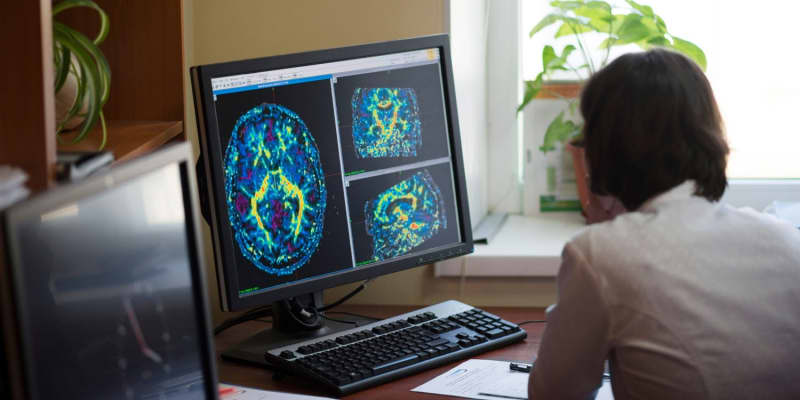
Anorexia nervosa is one of the most deadly psychiatric conditions, with a recovery rate of less than half of those affected. Research over the past decade has utilized functional magnetic resonance imaging (fMRI) to explore how this disorder alters brain connectivity.
These studies, however, often suffered from small sample sizes that yielded inconsistent results and limited reliability. Prior studies identified altered connectivity in regions like the insula and anterior cingulate cortex but could not comprehensively map connectivity across the entire brain due to these limitations.
“Anorexia nervosa is a serious eating disorder in which the fear of gaining weight leads to excessive dieting and exercise, resulting in significantly low body weight, with a very high long-term mortality rate of 18%,” said senior study author Yoshiyuki Hirano, a professor and vice director of the Research Center for Child Mental Development at Chiba University and professor and associate dean of the United Graduate School of Child Development at Osaka University.
“Despite this, the pathophysiology of the disease is poorly understood and effective treatments have not been developed, as it is not yet clear what brain abnormality causes the disorder. To overcome this situation, a number of studies have investigated resting-state functional connectivity using fMRI, which can examine brain activity.”
“However, the sample size of previous studies was less than 30 subjects per group, resulting in many inconsistencies and discrepancies in results between studies due to a lack of reliability and only analyzing functional connectivity between some brain regions. Therefore, we considered it necessary to conduct functional connectivity analyses between all regions of the whole brain in a multicentre study with a sufficient sample size, and to comprehensively elucidate the abnormalities in brain function occurring in the symptoms of anorexia nervosa with a high degree of reliability.”
Conducted across five Japanese hospitals, the study included 114 female anorexia patients and 135 healthy controls. To address potential biases and variations inherent in multi-site studies, all participants underwent the same diagnostic interviews and psychological assessments, and MRI scans were conducted using the same type of 3.0 Tesla MRI scanners across all locations. The research was conducted by Hirano and first author Yusuke Sudo, a research fellow at the Research Center for Child Mental Development at Chiba University, along with 32 other co-authors.
The researchers identified a total of 45 distinct alterations in resting-state functional connectivity when comparing individuals with anorexia nervosa compared to healthy controls. Resting-state functional connectivity refers to the brain activity patterns observed when an individual is not engaged in any specific task, revealing how various regions of the brain communicate and coordinate with each other during rest.
The results indicated that connectivity was notably stronger in areas involving the rostral prefrontal cortex, particularly linked to the dorsolateral prefrontal cortex. This region is crucial for executive functions such as decision-making and cognitive control, which are often implicated in the pathological eating behaviors observed in anorexia nervosa. The enhanced connectivity here could relate to the heightened control over food intake and obsessive behaviors characteristic of the disorder.
Conversely, weakened connectivity was prevalent in areas like the cerebellum and the temporal lobes, as well as between the anterior cingulate cortex and the thalamus. The diminished connectivity within the temporal lobe and between these critical areas could be associated with the emotional and cognitive dysregulation commonly observed in anorexia nervosa. For instance, the weaker connectivity between the anterior cingulate cortex and the thalamus might contribute to difficulties in cognitive flexibility and set-shifting, which are known challenges in anorexia nervosa.
The reduced connectivity in the cerebellum, an area traditionally associated with motor control but also known to contribute to cognitive processing, might relate to the disrupted perception of body image and the altered eating behaviors characteristic of the disorder.
“The patients with anorexia nervosa showed a more extensive reduction in functional connectivity than expected, particularly between the cerebellum and the cerebrum,” Hirano told PsyPost. “On the other hand, there was stronger activity in the dorsolateral prefrontal cortex, a brain region responsible for the control of thought and behaviour that is found to be weakened in depression.”
The researchers further differentiated between the two main subtypes of anorexia: the restricting type and the binge/purge type. The findings revealed distinct connectivity patterns between these subtypes, suggesting possible neural signatures that could help in categorizing and treating the subtypes more effectively. For instance, the restricting type was linked to stronger connectivity between the right lingual gyrus and the right supracalcarine cortex and between the left temporal occipital fusiform cortex and the medial part of the visual network compared to the binge/purge type.
These findings suggest that anorexia nervosa is characterized by a complex pattern of both hyperconnectivity and hypoconnectivity across various brain networks, indicating a disrupted balance in the neural circuits that regulate eating behavior, emotional responses, and cognitive control. The presence of distinct connectivity patterns between subtypes of anorexia nervosa further suggests that these neural signatures could potentially aid in more tailored and precise diagnostic and therapeutic strategies.
“The fact that patients with anorexia nervosa do not stop restricting their diet and stubbornly refuse to accept persuasion from those around them, even after reaching an obviously low weight and damaging their health, is sometimes mistakenly believed to be due to personality bias or because they want to do so,” Hirano explained. “In reality, however, as shown in the present study, the brain function of patients with anorexia nervosa is significantly altered compared to normal subjects, resulting in abnormal eating behaviour control, body image disorders, excessive cognitive control over emotions and impaired social skills.”
These alterations in brain function “can lead to a vicious cycle that forces them to continue restricting their diet,” Hirano added. “Problematic behaviors are considered to be symptomatic of changes in brain function, and supporters are required to be sympathetic to the patient’s fears and anxieties, while persistently encouraging improvement in their nutritional status.”
Despite its strengths, the study has limitations. It was unable to determine whether the observed connectivity changes were causal factors in anorexia development or consequences of the disorder.
“This study was cross-sectional, so it could not determine whether the rsFCs that showed group differences were related to anorexia nervosa development or reflected temporal changes in brain function due to starvation,” Hirano explained. “Therefore, to better elucidate the brain dysfunctions involved in the development of anorexia nervosa, we are currently carrying out a cohort study investigating changes in the brain before and after treatment.”
The end goal is to reveal the “brain dysfunctions involved in the development and maintenance of anorexia nervosa, leading to the development of treatments such as pharmacotherapy, psychotherapy and neuromodulation that target these brain dysfunctions,” the researcher said.
The study, “Comprehensive elucidation of resting-state functional connectivity in anorexia nervosa by a multicenter cross-sectional study,” was authored by Yusuke Sudo, Junko Ota, Tsunehiko Takamura, Rio Kamashita, Sayo Hamatani, Noriko Numata, Ritu Bhusal Chhatkuli, Tokiko Yoshida, Jumpei Takahashi, Hitomi Kitagawa, Koji Matsumoto, Yoshitada Masuda, Michiko Nakazato, Yasuhiro Sato, Yumi Hamamoto, Tomotaka Shoji, Tomohiko Muratsubaki, Motoaki Sugiura, Shin Fukudo, Michiko Kawabata, Momo Sunada, Tomomi Noda, Keima Tose, Masanori Isobe, Naoki Kodama, Shingo Kakeda, Masatoshi Takahashi, Shu Takakura, Motoharu Gondo, Kazufumi Yoshihara, Yoshiya Moriguchi, Eiji Shimizu, Atsushi Sekiguchi, and Yoshiyuki Hirano.

