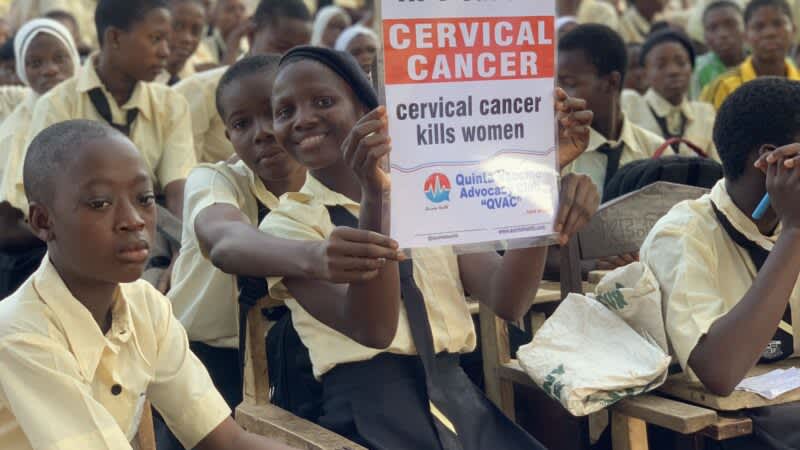
Quinta Health's vaccine advocacy for secondary schools (QVACS). Photo provided by Dr. Adewumi Babatunde, used with permission.
Sub-Saharan Africa, Central America and South-East Asia have the highest rates of cervical cancer incidence and mortality in the world. According to the World Health Organization (WHO), cervical cancer is the fourth most common cancer in women globally. In Nigeria, it is the third most common and the second most frequent cause of cancer deaths among women aged between 15 and 44 years. Current estimates indicate that every year 12,075 new cases and about 8,000 deaths are attributed to cervical cancer.
However, the tragedy of cervical cancer could easily be prevented and can be treated successfully if detected early. More than 95 per cent of cervical cancer cases worldwide are due to persistent infection with the sexually transmitted human papillomavirus (HPV), which most sexually active women and men will pick up at some point in their lives.
The HPV vaccine, when offered at an early age to girls, dramatically reduces cervical cancer rates later in life by almost 90 per cent.
Because of the growing concern around cervical cancer, Nigerian doctor/public health physician and founder of Quinta Health, Dr. Adewumi Babatunde who works as a senior registrar in public health at the Federal Medical Center in Abeokuta, south-west Nigeria spoke to Global Voices about his advocacy for cervical cancer screening and the importance of HPV vaccination.
Pamela Ephraim (PE): Dr. Babatunde, tell us why you advocate for this.
Dr. Adewumi Babatunde (AB): I have been advocating for cervical cancer since 2016. I began during my National Youth Service Corp (NYSC) and then later founded my own organization, Quinta Health, in 2017. My organization has been able to screen about 8,000 women for cervical cancer. We’ve been able to treat about 750 women for cervical dysplasia, delivered 500 doses of the HPV vaccine, and we have reached millions of women through different media: television, radio, social media — Instagram, Twitter, TikTok, Facebook and all that, educating them about cervical cancer. My love for this stems from the fact that cervical cancer is the second leading cause of cancer deaths among women in Nigeria. Nigeria has the highest burden of cervical cancer in Sub-Saharan Africa, coupled with the fact that I lost someone who was close to me to cervical cancer and I discovered that this cancer can actually be prevented. It is one of those few cancers that you can beat your chest if you do some things like vaccination, screening and treatment; eventually, if you’re positive, you will not have the cancer. I saw that this is something we can do in Nigeria and I decided to put my weight behind it.
PE: Beyond social media, where else have you advocated and what has the response(s) been like?
AB: My advocacy for cervical cancer screening goes beyond social media. Yes, we do on social media but I had already started working on the ground before social media. We’ve gone to churches, mosques, marketplaces, schools, and secondary schools; we’ve gone to universities and NYSC camps to advocate. We’ve been to practically everywhere you can find a woman to create awareness about cervical cancer because we know one of the key things to do is to first create awareness and let people know that there is something that can be done and there is a disease. A lot of people do not know. They attribute it to several other things — maybe, the act of God and all that but when people have this information, that is the first thing you can actually do to empower them. We’ve been to almost all the six geo-political zones in Nigeria to advocate by ourselves and in conjunction with other people.
The response has been fantastic. Lots of people say they do not even know about this cancer, so a lot of people want to learn more. A lot of people ask questions on social media. Interesting questions, including how they can get screened and vaccinated. And these questions have been keeping me going because the response has actually been really fantastic.
PE: Do you think getting HPV vaccines is a must?
AB: Everybody should get the HPV vaccine, both men and women. I wouldn’t say it is compulsory, but it is necessary because apart from cervical cancer, the HPV vaccine prevents against penal cancer, anal cancer, throat cancer, cancers of the head and neck, and also prevents genital warts, which are actually not cancer itself. But it's very important that everybody gets this vaccine because it helps to protect everybody from this cancer, and creates like a herd immunity. This means when a significant number of people in a place are vaccinated, this would help to build protection. So you’re protecting yourself against the other person also. Countries like the UK and Australia are vaccinating a lot of people and they’re getting good results. There was a study done in the UK that says 90 percent of the women who were vaccinated and followed up did not develop cervical cancer. So it is very important. I wouldn't say it's a must, but it is very important and necessary because you can't force vaccines on people, but the awareness should go far and wide that this vaccine can work magic in protecting against cancer.
PE: There has been a lot of debate about giving young women the vaccine. Are there any cons to taking the vaccine?
AB: There are concerns about every vaccine and all drugs. People have a right to their opinions but in the medical profession, we deal with facts and figures. The World Health Organization has certified the vaccines safe and effective. The FDA has certified it safe and effective, NAFDAC has done the same. Independent studies have also shown that the concerns linked to the vaccines aren’t related to the vaccines. There are lots of misconceptions like “it would cause infertility”; “it’s a ‘mark of the beast,” and so on. All of them are false. Millions of doses of the vaccines have been delivered in Nigeria, and has anyone heard reports of any serious issues?
Cervical cancer elimination
In England, nationwide vaccination against HPV began in 2008. A 2021 study00501-0/fulltext) estimated the programme had successfully almost eliminated cervical cancer in women born since September 1, 1995.
The WHO aims to eliminate cervical cancer as a public health problem if every country should meet the 90–70–90 targets by 2030. The targets depend on the three key pillars of vaccination: 90 percent of girls fully vaccinated with the HPV vaccine by the age of 15; screening: 70 percent of women screened using a high-performance test by the age of 35, and again by the age of 45; treatment: 90 percent of women with pre-cancer treated and 90 percent of women with invasive cancer managed.
In October 2023, Nigeria’s Federal Ministry of Health, through the National Primary Health Care Development Agency, with support from Gavi, the Vaccine Alliance, the United Nations Children's Fund (UNICEF), the World Health Organisation (WHO), and other partners rolled out free HPV vaccines for girls between the ages of nine and 15.
Nigeria’s coordinating minister of health and social welfare, Prof. Muhammad Pate, recently disclosed that about 4.95 million girls aged nine to 14 had been vaccinated against the Human Papillomavirus in the first phase of the vaccination across 15 states and the federal capital territory.
The second phase of the HPV vaccine rollout began on May 27 and will encompass the remaining states.
Written by Pamela Ephraim
This post originally appeared on Global Voices.
