A recent study published in Frontiers in Psychology investigates the relationship between psilocybin, mindfulness, mystical-type experiences, and serotonin receptors in the brain. Following participants for three months after a dose of psilocybin, the new findings indicate that when taking psilocybin, those who report mystical-type experiences are more likely to have increased trait mindfulness. In addition, those who took psilocybin had mystical experiences and became more mindful and saw less activity in the amygdala serotonin 2A receptors (5-HTR).
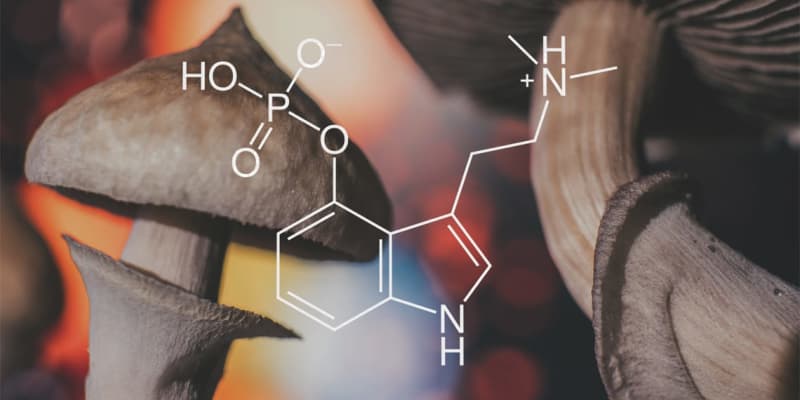
Psilocybin is a naturally-occurring psychedelic compound found in certain species of mushrooms. It has been used traditionally by indigenous cultures around the world for centuries in spiritual and psychological healing ceremonies. The compound was made famous in the 1960s counterculture movement; however, its therapeutic potential has come into focus in recent years.
Researcher Anna Søndergaard and her colleagues acknowledge the many potential applications of psilocybin, including as treatments for depression, obsessive-compulsive disorder, anxiety, alcohol abuse, and smoking. For those without illness or addiction, an earlier but smaller study found increases in trait mindfulness after a dose of psilocybin.
Søndergaard and her colleagues were curious to discover if enhanced trait mindfulness would continue over time, what (if any) was the relationship between mystical experiences when taking psilocybin, and finally, what role 5-HTR has to play in the development of mystical experiences or trait mindfulness. The study defines trait mindfulness as “the awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to the unfolding of experience moment by moment.”
The study included 39 participants recruited from a database of individuals willing to take psilocybin and undergo neuroimaging. In addition, they were screened for medical issues, pregnancy, and other drugs. Phase one of the study included providing each participant with a dose of psilocybin appropriate for their weight. More than ½ of the participants were either in a PET scan or an MR scanner. The remainder were in a comfortable room.
Six hours after the administration of the psilocybin, participants took a mystical experience questionnaire., which asked about things like feeling a sense of unity, ecstasy, losing your sense of time, or feeling like the experience could not be described. Finally, before and three months after the dose of psilocybin, participants took the Mindful Attention and Awareness Scale.
Statistical analysis revealed an 8.1% increase in trait mindfulness from before taking psilocybin to three months after. Furthermore, compared to the results of the mystical experience questionnaire, it was discovered that those who reported more intense mystical experiences also had higher trait mindfulness scores. The brain scans also identified less binding activity at 5-HTR in the right side of the amygdala.
Concerning this finding, the research team stated, “the right amygdala may be more involved in mindfulness than the left amygdala…further studies need to explore the role of serotonin for individual differences in response to psychedelic administration.”
The researchers acknowledged some limitations. These include the three-month gap between the administration of the drug and the final measure of mindfulness. Participants could have been pursuing a mindfulness practice during this time. The study also had no blind control group.
The research team does not believe these limitations diminish the value of their work. Instead, they suggest the following: “psilocybin and the mystical-type experience could have mindfulness-enhancing capacities and may potentially work in synergy with mindfulness-based forms of therapies in a clinical setting.”
The study, “Lasting increases in trait mindfulness after psilocybin correlate positively with the mystical-type experience in healthy individuals”, was authored by Anna Søndergaard, Martin Korsbak Madsen, Brice Ozenne, Sophia Armand, Gitte Moos Knudsen, Patrick McDonald Fisher, and Dea Siggaard Stenbæk.
