A neuroimaging study on U.S. military veterans showed that the amygdala region of the brain of veterans with post-traumatic stress disorder (PTSD) showed lower reactivity to pain compared to the same region of the brain of veterans without PTSD.
Patterns were unique to this region of the brain and the researcher link this to emotional numbing, a restriction in the capacity of an individual to experience emotions. Other brain regions associated with processing pain were unaffected.
The study was published in Neuropsychopharmacology.
PTSD is a disorder that sometimes develops in people who have experienced a traumatic event or a series of traumatic events. While most people will experience substantial stress reactions to such events, these reactions will sometimes persist over time and lead to this disorder.
The most well-known symptoms of PTSD include intrusive memories of the traumatic event, the so-called flashbacks, bad dreams and frightening thoughts, but symptoms also include higher pain tolerance, emotional numbing and many others.
Reactivity to pain and PTSD are often seen as associated. Traumatic events leading to PTSD typically involve pain or a threat of pain. One characteristic of PTSD is the “high threshold – high response” pattern to pain, a tendency to not respond to pain of low intensity, but react very strongly when the pain becomes too much.
This is similar to the response pattern to emotional stimuli of people with PTSD known as emotional numbing. Emotional numbing refers to the restricted capacity to experience either positive or negative emotions accompanied by proneness to extreme reactions to highly negative stimuli.
Building on previous studies that showed changes to reactivity of certain brain regions in people with PTSD, Nachshon Korem and his colleagues wanted to study how brain reactivity to pain might be affected by this disorder. They carried out two studies of U.S. military veterans.
The first study involved 44 veterans, one group meeting diagnostic criteria for PTSD and the other group was without a PTSD diagnosis (combat controls). All participants completed an assessment of emotional numbing. The second study was a conceptual replication of the first with 71 veterans.
Participants went through a fear conditioning task in which exposure of colored squares was paired with electric shocks to the inner wrist of the participant’s dominant hand. During this task, participants underwent magnetic resonance imaging of their brains and researchers also collected data on skin conductance responses using electrodes attached to the first and second fingers of each participant’s nondominant hand.
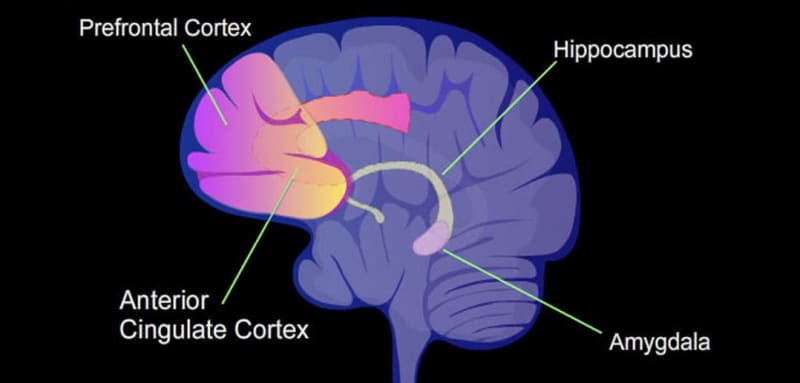
“In both samples, we found an overall reduction in amygdala (but not insula) responsivity to mild pain in the PTSD group, compared with Combat Controls,” the study authors report. The size of the reduction was linked to the severity of emotional numbing in the person – the higher the emotional numbing, the lower the reactivity of the amygdala brain region.
The researchers found that this pattern was unique to the amygdala region of the brain and that it was not detected in the insula, a brain region pivotal in the processing of pain.
“Amygdala response to pain is lower in individuals with PTSD, and is associated with emotional numbing symptoms. Lower amygdala reactivity to mild pain may contribute to the “all-or-none” reaction to stressful situations often observed in PTSD,” the researchers conclude.
The study sheds light on important neural mechanisms behind some of the psychological changes observed in persons with post-traumatic stress disorder. However, authors note that both samples consist solely of veterans and males, limiting how much results can be generalized to females and males who were not part of the military.
The study, “Emotional numbing in PTSD is associated with lower amygdala reactivity to pain”, was authored by Nachshon Korem, Or Duek, Ziv Ben-Zion, Antonia N. Kaczkurkin, Shmuel Lissek, Temidayo Orederu, Daniela Schiller, Ilan Harpaz-Rotem, and Ifat Levy.
