A recent study published in the New England Journal of Medicine suggests that psilocybin therapy may offer therapeutic benefits for patients with treatment-resistant depression. When administered alongside psychological support, a 25 mg psilocybin dose reduced depression scores among treatment-resistant patients. However, adverse effects were reported, and further clinical trials are needed.
Clinical depression is typically treated with a combination of anti-depressant medication and psychotherapy. While most patients experience a reduction in symptoms with anti-depressants, a subset of people fail to respond to the medication. A case that does not respond to two courses of anti-depressants is referred to as treatment-resistant depression.
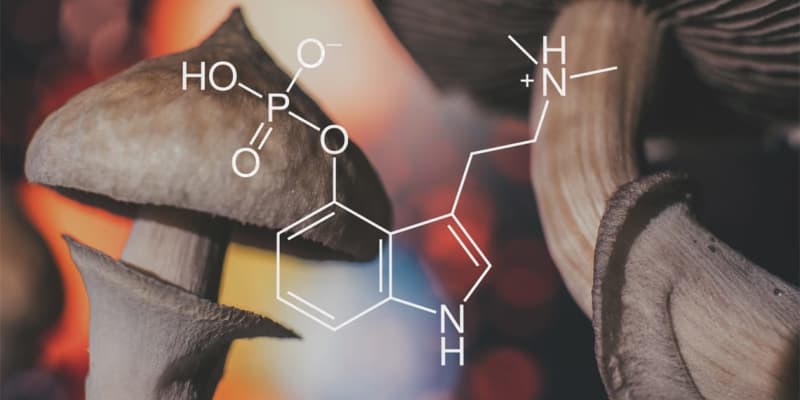
Preliminary studies have suggested that psilocybin — a psychedelic compound found in certain species of mushrooms — may have antidepressant properties. In their recently-published study, researchers Guy M. Goodwin and his colleagues explored its potential to treat depression among people who are resistant to usual treatment.
“The potential of psychedelics in mental health has been investigated by scientists for many years, but only recently has research moved to larger scale studies,” explained Goodwin, the chief medical officer at COMPASS Pathways.
“These large trials are needed to demonstrate treatments are safe and effective, receive regulatory approvals, and get them to people who urgently need new options. We focus on areas of unmet need in mental health, for example treatment-resistant depression, which affects 100 million people globally.”
“We have just begun a phase 3 programme in treatment-resistant depression, which is the largest-ever clinical trial of psilocybin therapy globally, and we’re also studying COMP360 psilocybin therapy in post-traumatic stress disorder and anorexia nervosa.”
The researchers conducted a double-blind, randomized clinical trial among 233 patients diagnosed with treatment-resistant depression. The study was conducted at 22 sites in 10 different countries. For 3-6 weeks leading up to the study, participants tapered off any antidepressants they were taking and met with a therapist to prepare for the trial. Participants were then randomly assigned to receive either a 25 mg, a 10 mg, or a 1 mg dose of psilocybin. The 1 mg dose served as a control condition.
After the treatment, participants were followed for 12 weeks. The day after the treatment and one week after treatment, the participants attended therapist-led integration sessions to help them reflect on the psilocybin experience. Participants also completed assessments of depression over the phone at various time points throughout the study.
Goodwin and his team analyzed changes in participants’ depression scores, comparing the groups who received 25 mg and 10 mg of psilocybin to the control group. The results revealed that from baseline to week 3, the 25 mg group showed improvements in their depression scores that significantly exceeded changes in the 1 mg group. Change in depression scores was no different between the 10 mg and 1 mg groups.
“We saw positive results in a particularly difficult to treat type of depression – treatment-resistant depression – where patients have tried at least two antidepressant treatments without success,” Goodwin told PsyPost.
“Our study showed that after a single 25mg dose of COMP360 psilocybin therapy with psychological support, approximately 30% of patients were in remission at three weeks, and we saw effects lasting for up to three months.”
Notably, adverse events were reported in all groups, the most common being headaches, nausea, dizziness, and fatigue. Reports also included suicidal ideation and self-injurious behavior, and these events were more common among those who took 25 mg or 10 mg compared to 1 mg.
Limitations of the study include that the sample was not ethnically diverse, with 92% of participants being White. Additionally, the study did not assess whether participants could correctly guess which dose of psilocybin they received, which means that placebo effects cannot be entirely ruled out.
Overall, the findings suggest that a single dose of 25 mg of psilocybin — but not 10 mg — can improve depression symptoms among people with treatment-resistant depression when administered alongside therapy. Nevertheless, the adverse events are cause for concern, particularly the reports of worsening suicidality.
“We are about to start the world’s first ever phase 3 pivotal programme of psilocybin therapy in treatment-resistant depression,” Goodwin said. “Our phase 3 programme will seek to validate our phase 2b results published in the New England Journal of Medicine, and also investigate if a second dose of COMP360 psilocybin can increase rates of treatment response seen in the phase 2b study.”
The study, “Single-Dose Psilocybin for a Treatment-Resistant Episode of Major Depression”, was authored by G.M. Goodwin, S.T. Aaronson, O. Alvarez, P.C. Arden, A. Baker, J.C. Bennett, C. Bird, R.E. Blom, C. Brennan, D. Brusch, L. Burke, K. Campbell‑Coker, R. Carhart‑Harris, J. Cattell, A. Daniel, C. DeBattista, B.W. Dunlop, K. Eisen, D. Feifel, M.K. Forbes, H.M. Haumann, D.J. Hellerstein, A.I. Hoppe, M.I. Husain, L.A. Jelen, J. Kamphuis, J. Kawasaki, J.R. Kelly, R.E. Key, R. Kishon, S. Knatz Peck, G. Knight, M.H.B. Koolen, M. Lean, R.W. Licht, J.L. Maples‑Keller, J. Mars, L. Marwood, M.C. McElhiney, T.L. Miller, A. Mirow, S. Mistry, T. Mletzko‑Crowe, L.N. Modlin, R.E. Nielsen, E.M. Nielson, S.R. Offerhaus, V. O’Keane, T. Páleníček, D. Printz, M.C. Rademaker, A. van Reemst, F. Reinholdt, D. Repantis, J. Rucker, S. Rudow, S. Ruffell, A.J. Rush, R.A. Schoevers, M. Seynaeve, S. Shao, J.C. Soares, M. Somers, S.C. Stansfield, D. Sterling, A. Strockis, J. Tsai, L. Visser, M. Wahba, S. Williams, A.H. Young, P. Ywema, S. Zisook, and E. Malievskaia.
