Researchers have uncovered a potential preventative treatment for breast cancer, other than surgery, in women with BRCA1 and BRCA2 gene mutations.
If it proves successful in mouse models, human clinical trials of this early intervention method will be carried out.
It follows work by the University of Cambridge, European Bioinformatics Institute (EMBL-EBI) and Wellcome Sanger Institute to create the world’s largest catalogue of human breast cells.
This revealed early cell changes in healthy carriers of BRCA1 and BRCA2 gene mutations.
While everyone carries these genes, mutations in them - which can be inherited - are known to increase the risk of breast and ovarian cancer.
The researchers found the immune cells in breast tissue of healthy women with these gene mutations show signs of a malfunction known as ‘exhaustion’.
It suggests the immune cells cannot clear out damaged breast cells, which can eventually develop into breast cancer.
Exhausted immune cells are usually only found in late-stage tumours. They have never been reported in non-cancerous breast tissues at such scale before.
But the finding raises the prospect of using existing immunotherapy drugs as an early intervention to prevent breast cancer developing in carriers of BRCA1 and BRCA2 gene mutations.
Cancer Research UK has granted the researchers a ‘Biology to Prevention Award’ to trial the preventative approach in mice.
This will be key, as existing drugs have serious side effects and the testing in mice will help to find a safe dosage before a pilot clinical trial in women with the BRCA mutations.
“Our results suggest that in carriers of BRCA mutations, the immune system is failing to kill off damaged breast cells - which in turn seem to be working to keep these immune cells at bay,” said Prof Walid Khaled in the University of Cambridge’s Department of Pharmacology and Wellcome-MRC Cambridge Stem Cell Institute, senior author of the report.
“We’re very excited about this discovery, because it opens up potential for a preventative treatment other than surgery for carriers of BRCA breast cancer gene mutations.
“Drugs already exist that can overcome this block in immune cell function, but so far, they’ve only been approved for late-stage disease. No-one has really considered using them in a preventative way before.”
Women at increased risk of breast cancer are offered risk-reducing surgery, in which both breasts are removed. But that can be a difficult decision for young women to make and impact their body image and sexual relationships.
“The best way to prevent breast cancer is to really understand how it develops in the first place. Then we can identify these early changes and intervene,” said Prof Khaled.
“Late-stage breast cancer tends to be very unpredictable and hard to manage. As we make better and better drugs, the tumours just seem to find a way around it.”
For the study, reported in the journal Nature Genetics, samples of healthy breast tissue were collected from 55 women of different ages and more than 800,000 cells were catalogued, including every type of breast cell.
The Human Breast Cell Atlas created - part of the wider effort to create a complete Human Cell Atlas \- contains a large amount of data on other risk factors for breast cancer including Body Mass Index (BMI), menopausal status, contraceptive use and alcohol consumption.
Other researchers can now freely access this and add to it.

“We’ve found that there are multiple breast cell types that change with pregnancy, and with age, and it’s the combination of these effects - and others - that drives the overall risk of breast cancer,” said Austin Reed, a PhD student in the University of Cambridge’s Department of Pharmacology and joint first author of the report.
“As we collect more of this type of information from samples around the world, we can learn more about how breast cancer develops and the impact of different risk factors - with the aim of improving treatment.”
Breast cancer is in fact many diseases and many genetic variations can lead to it, with genetic risk interacting with other risk factors, creating a complicated web to untangle for scientists.
We know the likelihood of breast cancer increases with age, but also that this risk is greatly reduced by pregnancy early in life. Age-associated risk is greatly increased for carriers of the BRCA1 and BRCA2 gene mutations.
The work to characterise the different cell types in the human breast under different physiological states will help us understand the interaction of these risk factors.
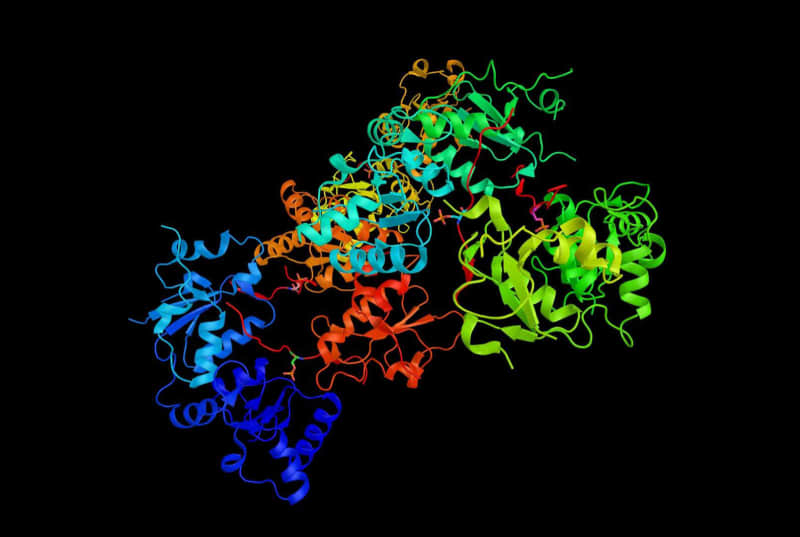
Single cell RNA sequencing - which tells us which genes are switched in in individual cells - was used to characterise the different cell types and states. While almost all of our cells have the same set of genes, only a subset is switched on in each cell.
Dr Sara Pensa, senior research associate in the University of Cambridge’s Department of Pharmacology and joint first author of the study, added: “Breast cancer occurs around the world, but social inequalities mean not everyone has access to treatment. Prevention is the most cost-effective approach. It not only tackles inequality, which mostly affects low-income countries, but also improves disease outcomes in high-income countries.”
The research was primarily funded by the Medical Research Council and Cancer Research UK, with breast tissue samples provided by the Breast Cancer Now tissue bank.
